[ad_1]
Spiritual leader Sadhguru Jaggi Vasudev has been discharged from the Indraprastha Apollo Hospitals in Delhi today after his successful emergency brain surgery on March 17. The mystic and Yogi had suffered multiple bleedings in the brain before he was hospitalised. He suffered from persistent and severe headaches for several weeks. Brain bleeding, also known as intracranial haemorrhage, occurs when blood vessels in the brain rupture, leading to blood leakage into surrounding tissues. This can result in neurological complications or even death. Immediate medical attention is important to address this serious condition. (Also read: Sadhguru Jaggi Vasudev discharged from hospital after brain surgery)

“The doctors have expressed satisfaction with his recovery and healing. Sadhguru, even as he is recovering, has maintained the same spirit. His commitment to the global good, his sharp mind and his sense of humour are all intact. I think this is good news for all the millions of people who have been enquiring about his health,” said Dr Sangita Reddy, Joint Managing Director – Apollo Hospitals Group.
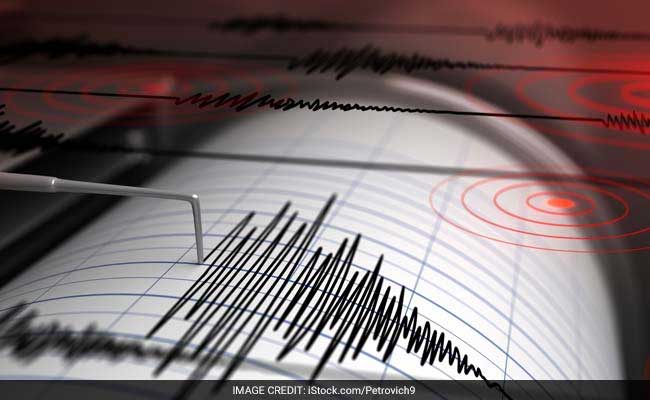
What is brain bleeding?
Brain bleedings occurs as a result of rupturing of blood vessels in brain. It can be in any part of brain or on surface.
“Extra dural (EDH) or subdural hematoma (SDH) is due to trauma and rarely due to side effects of blood thinners. Haemorrhage inside the brain is due to high blood pressure and rupture of blood vessel. It can be due to rupture of vascular malformation like AVM, aneurysm, or dural AVF,” explains Dr Rahul Gupta, Director Neuro Surgery, Fortis Hospital, Noida.
Elaborating on the treatment strategies in case of a large haemorrhage, Dr Gupta says “they need surgery and evacuation as a life-saving measure. The angiography of the brain is needed to diagnose any vascular malformation and that is treated accordingly. Vascular malformation can be treated by open surgery like clipping of aneurysm or excision of AVM or can be treated by embolisation in Neurocathlab by endovascular methods like coiling, stenting, glue insertion, or intraluminal device placement.”
“In elderly, trivial trauma may lead to small SDH, which may gradually expand and become chronic SDH. This may require burr holes and evacuation if the patient becomes symptomatic,” the expert adds.
Symptoms of brain bleeding
Sudden and severe headache is a telltale sign of a brain haemorrhage in most cases and may be associated with high blood pressure.
“Brain haemorrhage presents as sudden severe headache in 80 per cent cases. This headache may be associated with loss of consciousness, vomiting, or limb weakness. Rarely, there can be a seizure or blurring of vision. Uncommonly, there can be repeated minor headaches, which may indicate repeated minor bleeding. These are called sentinel bleeds. They may be associated with high blood pressure and are like warning signs,” says Dr Gupta.
How to diagnose brain bleeding
Timing is of essence when it comes to diagnosing brain bleeds and CT scan must be performed immediately to detect them.
“CT scan brain is the most important investigation to detect brain bleeding. Sometimes MRI and angiography are needed. Surgery may be needed in one third patients hence patient should be shifted to hospital, immediately where all facilities are available. In these cases, time is of great importance and every passing minute is valuable. Any delay in treatment can lead to death of patient. Of all the patients who need surgery, about 50 per cent have a good outcome if treated aggressively in a good hospital. Other patients may remain bedridden or dependent on care giver. About 10% may not survive. In the last few decades with advent of advanced care in multispeciality hospitals and good operative and ICU facilities, results have improved drastically,” concluded the expert.
[ad_2]
Source link